Social Prescription
Learn about evidence, history, benefits, and resources for integrating social prescription into your practice. Use the following links to navigate to any section.
What is Social Prescription?
Social prescribing aims to shift away from just treating physical symptoms and move towards promoting broader well-being through the creation of healthier and more connected communities. For an individual, it can help to reduce mental health issues, feelings of loneliness, and overall mental wellbeing and functioning while fostering stronger social connections and empowering individuals to take an active role in their health. For communities, it reduces pressure on healthcare services, promotes local resources, and strengthens social cohesion.
It is thought that about 20% of patients consult their general practitioner primarily about social issues. Social prescription is gaining popularity due to the aging population, increasing complexity of health and social needs, and increasing demands on services. Research in Canada on social prescription is also growing. There is a large potential for social prescription to be adopted by community leaders, researchers, and future health professionals.
The essence of social prescribing connects individuals to community services, such as programs and activities held in community senior centres. Activities include exercise groups, art therapy, or social clubs to improve overall well-being by minimizing social isolation. A family physician, nurse practitioner, or another allied health professional can refer an older adult experiencing social isolation to a community senior centre.
History of Social Prescription
Social prescription originated in the United Kingdom in the 1980s. Inspired by its growth in the UK and other countries, it has been embraced in Canada, the United States and around the world. Social prescription initially began in underprivileged areas in populations who had complex physical and mental health problems, low socioeconomic status, and hectic lifestyles. These were often populations that required social solutions alongside medical treatment. Over time, social prescription has been used in older populations with an aim to reduce feelings of loneliness, improve levels of physical activity, and overall mental well-being.
In 2018, a year-long pilot project titled Rx: Community - Social Prescribing, was conducted in Ontario to gain a better understanding of social prescription and furthered the use of it provincially. There are now initiatives underway in every province, with some focusing on particular populations such as caregivers, older adults and Black communities, and some focus on specific interventions including food, arts and culture, and physical activity.
Benefits of Social Prescription
The benefits of social prescribing include, but are not limited to:
- Decreased experiences of loneliness. Provides space to relax with friends and have a moment for respite.
- Building connections to the community and peer supports:
- Provides meaning and a sense of purpose, fosters trust, improves ability to cope with life stress.
- Improved health and well-being, optimism for life, and an elevated mood through building friendships and engagement in meaningful activities, sometimes acting as a needed distraction.
- Greater capacity to self-manage health through the development of new coping skills and social supports with peer-learning and shared experiences.
- Strengthens community ties and improve identity within a community.
- Potential for fewer hospital visits and decreased length of stay, decreased reliance on primary care/healthcare services, and fewer repeat visits with primary care physicians.
- Individual empowerment to identify needs and to learn new ways to connect with what matters most.
- Efficiency for healthcare providers to direct individuals to sources to address non-medical needs.
Considerations When Implementing Social Prescription
A number of healthcare practitioners and researchers have begun calling out potential pitfalls of social prescription that make it hard to integrate into practice.
- Limited evidence to support the effectiveness of social prescription.
- The activities considered under the umbrella of social prescription are very diverse, as are the populations that are being targeted for intervention. This makes it difficult for researchers to find evidence proving the overall effectiveness of social prescription.
- Social prescription does not address the complex social and environmental factors that impact the most vulnerable people in our communities.
- It is not a solution for addressing the root causes of health inequities in our societies and instead places the responsibility of change on the individual.
- Accessibility and utilization barriers that limit individuals from accessing and benefiting from these programs.
- These barriers include can have travel-related time, costs, economic situations, finite program schedules, inconvenient timing.
- Lack of application/existence of needs assessment and clearly defined referral procedure.
- As there is no tool to identify the holistic needs of the individuals, it may make the referral process confusing and potentially time-consuming for family physicians or allied health professionals to do.
Organizations Related to Social Prescription
- The Canadian Institute of Social Prescribing (CISP) is a national collaborative anchored in the Canadian Red Cross. They are part of a global movement to bring community capacity and healthcare services together to enhance health and well-being. Their website raises awareness about social prescription in Canada, provides education sessions, offers connections with stakeholders to support program design, and promotes the latest research. CISP also advocates for practice and policy changes with government stakeholders to foster sustainable investments in social prescribing through community-based services.
- The Canadian Social Prescribing Student Collective (CSPSC) is a student-led organization that aims to educate future healthcare professionals across Canada on social prescription as an intervention strategy. They currently have seven groups at post-secondary institutions to build the social prescribing student movement. They represent Canada at the international level on the Global Social Prescribing Student Council.
- The Older Adult Centres’ Association of Ontario (OACAO) is a non-profit provincial organization and registered charity that develops services, resources and support for their network of over 230+ community-based older adult centers, seniors’ clubs/seniors’ councils and associate members. They share a strong commitment to ongoing liaison and advocacy with the Government of Ontario and other provincial associations in topics that impact older adult centers, SALCs and older adults.
OACAO aims to improve the quality and accessibility of resources, services, and support for community-based older adult centres to enhance community connectedness through activity and social engagement. They work as a liaison between government and provincial associations, acting as advocates to support the individuals using the older adult centres being funded. OACAO hosts workshops, webinars, and conferences, with additional information shared via newsletters and resources.
OACAO is also an advocate for social prescription both to the individual (e.g., expanding peer support, reducing the risk of hospitalization and/or social isolation) and the centre itself through supporting community outreach, engaging volunteers, and building membership. They also maintain micro-grants to support participating centres and reducing participation barriers.
OACAO supports several related programs:
- Links2Wellbeing
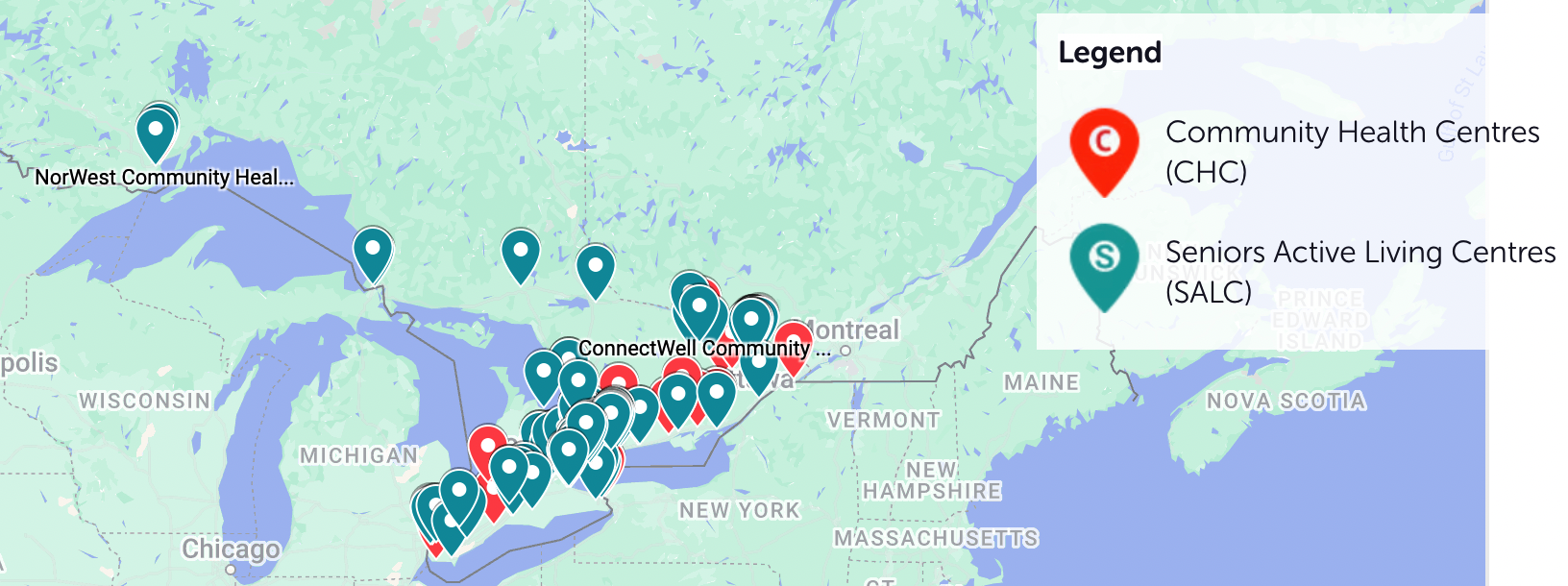
- This national social prescribing network started in 2021. It enables family physicians, nurse practitioners, and other allied health providers to make connections to programs/services offered by Senior Active Living Centres (SALCs) for older adults that are at risk of or experiencing social isolation.
- Over 90 centres are involved and over 1,500 social prescriptions have been provided in Ontario alone.
- Seniors’ Centre Without Walls (SCWW)
- SCWW’s goal is to remove barriers to a variety of programs and make them safe and easy for older adults to participate. They take a holistic approach to place consideration into a wide variety of potential barriers, including comfort levels, ability to use technology, and health concerns.
- Oasis is a model that offers programming for older adults living within a naturally occurring retirement community (NORC). A NORC is a community that has a naturally high density of older adult residents. These are not typically advertised as a ‘retirement community’ but can be a community that was designed to house a large concentration of older adults. The Oasis program falls on three pillars for healthy aging: nutrition, physical activity, and social engagement. These pillars are backed by evidence provided by the General Healthy Aging WHO initiative and the UN Decade of Healthy Aging Plan of Action. The program provides community kitchens and group meals for nutrition; group physical activity groups such as walking or line dancing; and social activities including games and crafts. The Oasis program receives funding from the Canadian Institute of Health Research to continue their longitudinal evaluation from 2021-2025. This is meant to have a better understanding of Oasis influence on healthy aging through decreasing social isolation.
- Some municipalities partner with organizations, such as the OACAO’s Links2Wellbeing program, to offer discounted or free local services and memberships for older adults at recreational centres. An example of this is the City of Waterloo. They are partnered with the Links2Wellbeing program to offer free social programs for older adults ages 55 and older referred for social isolation from a healthcare professional. Look into your local municipality to see if they are participating in any social prescription programs. It is important to make sure it specifies social prescription and that the program requires a prescription from a healthcare professional. Some municipalities have discounted memberships or programs for older adults which can be an option for socialization, but may not take part in a social prescription program.
- Community health and well-being networks include the University Health Network (UHN) in Toronto and the Canadian Mental Health Association (CMHA). UHN’s Social Medicine Program offers health equity initiatives for disadvantaged populations. CMHA facilitates a social prescribing program with Life After Fifty to provide clients an opportunity to connect with others in the community. Older adults must be referred by a healthcare provider.
Agencies in Ontario Practicing Social Prescription
Implementation of Social Prescription
There are different ways you can implement social prescription into your practice. By connecting with organizations and initiatives, such as Links2Wellbeing and OACAO, you can learn more about how to get involved with social prescribing in your area and how to make a referral.
At the micro level, we can work one-on-one with clients to provide a social prescription as a part of our recommendations if it suits their needs and goals. This can include connecting with their community, finding new occupations/rekindling their love for old occupations, and connecting them with programs that offer social prescription services.
At the meso level, we can advocate and assist in designing community programs in our local communities. OTs can play an important role in designing programs, applying for program funding, conducting research, and provide training to the staff within the community program. This may also look at forming new partnerships, such as with provincial or federal parks.
At the macro level, we can advocate for government funding for social prescription programs to ensure continued services. This can include conducting research to understand the effectiveness of programs in your area or working with an organization to advocate to social policy changes.
Future Recommendations for Social Prescription
To ensure that the benefits of social prescription are seen by clients, OTs must use their clinical reasoning to determine whether social prescriptions are the right fit. More research into social prescription, its benefits, pathways, and implementation are crucial to inform evidence-based practice.
As OTs implement social prescription, we must critically reflect and address the root causes of health inequities. In advocating for more comprehensive and long-term social interventions, we can begin to strengthen the effectiveness of social prescriptions for various populations. Advocacy should also continue to increase social prescription programs and access.
Additional Resources
Thank you to the second year student occupational therapists from Western University, in collaboration with OSOT's Retired Members Team, for developing this resource page.
